September is Sickle Cell Awareness Month. More than 100,000 Americans are diagnosed with sickle cell anemia, an inherited blood disorder that affects the shape of red blood cells, which carry oxygen to all parts of the body. In sickle cell anemia, some red blood cells are half-shaped, becoming rigid and sticky, which can slow or block blood flow and cause the patient to suffer.
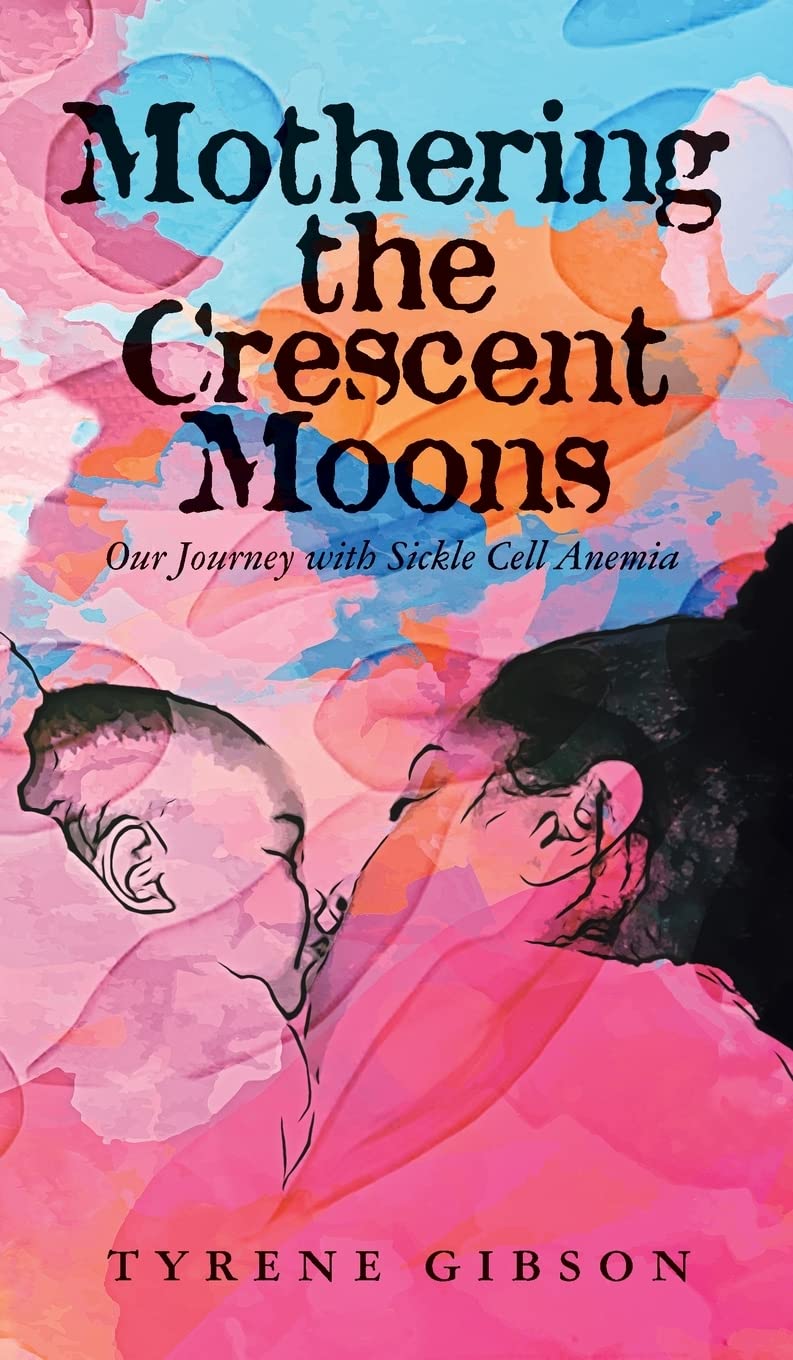 As a part of Sickle Cell Awareness Month, Tyrene Gibson, author of Mothering the Crescent Moons: Our Journey with Sickle Cell Anemia, and Erika Young, a microbiologist and sickle-cell survivor, discussed their stories about living and thriving with sickle cell disease.
As a part of Sickle Cell Awareness Month, Tyrene Gibson, author of Mothering the Crescent Moons: Our Journey with Sickle Cell Anemia, and Erika Young, a microbiologist and sickle-cell survivor, discussed their stories about living and thriving with sickle cell disease.
It was the 1970s when Erika Young learned she had sickle cell disease. “One of my pediatricians let me see my blood in the microscope. I was able to actually see the regular, healthy round cells compared to the sickle cell.” Like many at that time, her parents were unaware they were carriers of the trait. “My parents, of course, did not know they had the trait. During that day, they were not testing. So we found out they had the trait based on me having the disease.”
Erika was fortunate to have a doctor that was able to tell her more about the disease. “Dr. Zala Kafir was the first African American doctor that I had. He educated me more on the disease. He was the only physician to tell me that I still had a good percentage of my fetal hemoglobin left. At that time, it was like, between 12 and 14%, which he was surprised by. Fetal hemoglobin is essentially baby hemoglobin that’s more enriched and oxygenated, and you use you lose it early in life as soon as a child. So for me to have a high percentage of it left at eighteen years old, he said that may have helped me do as well as I had done.”
Unlike Erika Young’s parents, Tyrene Gibson, whose daughter has sickle cell disease, was made aware that she had the trait. “My brother and I were told by our pediatrician in Baltimore that we had the trait, and I knew that the trait came from my dad’s side of the family because he had indicated that his mother carried the trait.”
Despite knowing she had the trait, growing up, she never knew anyone who had sickle cell disease and therefore did not know what to expect when she was told that her daughter would have the disease while she was pregnant during her amniocentesis test. “I really didn’t know what to expect when they initially said to me that your daughter is going to come out with the disease. And my gynecologist and OB/GYN, you know, said that he would give me literature, but I should also speak to a doctor that specializes more in hematology and oncology and also interview a pediatrician since I was going to be having a baby that had the disease.”
Even after reading the literature, Tyrene was unprepared for just how much pain the disease would cause her daughter and how even doctors could be unprepared to deal with it, especially since there are only 56 sickle cell centers across the United States, leaving staff uneducated. “I feel as though every emergency room should have a protocol for sickle cell patients as soon as they come in. They should not have to wait for long periods of time. They should take them back immediately, get them hydrated until a doctor can see them. If they’re coming to the ER that that means that they’re in pain.”
Tyrene wishes that every doctor would realize that every patient with sickle cell is different. “I mean, when the doctor initially had said your child isn’t sick enough, I wanted to flip out. I said to myself, what do you mean? How sick do you need to be in order to go through a transplant?”
In many instances like this, doctors do not believe the pain crisis sickle cell patients are experiencing is severe enough for surgery, leading to increased painkiller prescriptions. The lack of education on sickle cell anemia was an important motivating factor for Tyrene, who wants to make sure we have conversations surrounding this disease. “I would like to see more people talking about it. Let’s have these conversations to make sure that you know whether you carry the trait or not carry. Hopefully, also to educate our clinicians, our doctors, our nurses with their training and how they’re being trained regarding sickle cell patients.”
If you would prefer a podcast version of the discussion you can listen to the full interview with Dr. Kendra Outler MD from Uzima Health and Wellness, Tyrene Gibson, author of Mothering the Crescent Moons: Our Journey with Sickle Cell Anemia; and Erika Young, a microbiologist and sickle cell survivor.
You can also watch the discussion in the video below.